- About Us
- Shoulders
- Shoulder injuries and conditions
- Acromioclavicular Joint Arthritis
- Acromioclavicular Joint Dislocations (Shoulder separation)
- Biceps Tendonitis
- Biceps Tendon Tear
- Calcific Tendonitis
- Collarbone Fracture
- Frozen Shoulder
- Shoulder Dislocations
- Labral Tears
- Pectoralis Major Rupture
- Proximal Humerus (Shoulder) Fractures
- Rotator Cuff Tears
- Shoulder Impingement
- Shoulder Joint Arthritis
- Shoulder Spur
- SLAP Tears
- Subacromial Bursitis
- Shoulder Surgery
- Acromioclavicular Joint Stabilisation
- Arthroscopic AC Joint Resection
- Arthroscopic (Keyhole) Labral Repair
- Arthroscopic (Keyhole) Rotator Cuff Repair
- Arthroscopic SLAP repair
- Biceps Tenodesis
- Broken Collarbone Surgery
- Latarjet Procedure
- Fixation of Proximal Humerus (Shoulder) Fractures
- Subacromial Decompression and Acromioplasty
- Reverse Shoulder Replacement
- Total Shoulder Replacement
- Case studies
- AC Joint Arthritis
- Broken Collarbone – Cycling accident
- Broken Collarbone – Scooter accident
- Shoulder Fracture – Complex Humerus Fracture
- Shoulder Fracture – Displaced Humerus Fracture
- Shoulder Fracture – Scooter accident
- Shoulder Fracture – Gardening
- Shoulder Fracture – Proximal Humerus
- Reverse Shoulder Replacement – Pain
- Reverse Shoulder Replacement – Shoulder Pain
- Rotator Cuff Tear
- Rotator Cuff Repair + Biceps Tenodesis
- Shoulder Dislocation – Latarjet
- Shoulder Dislocation – Instability
- SLAP Tear
- Total Shoulder Replacement
- Shoulder injuries and conditions
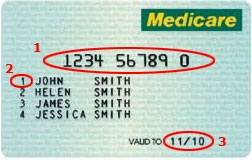
- Patient Info
- Articles
- Gallery
- Locations
- Contact