The key point is to remember which conditions in your shoulder are “time urgent” and which are not. Dr Pant will clearly outline this for you during your consultation.
Time urgent shoulder conditions
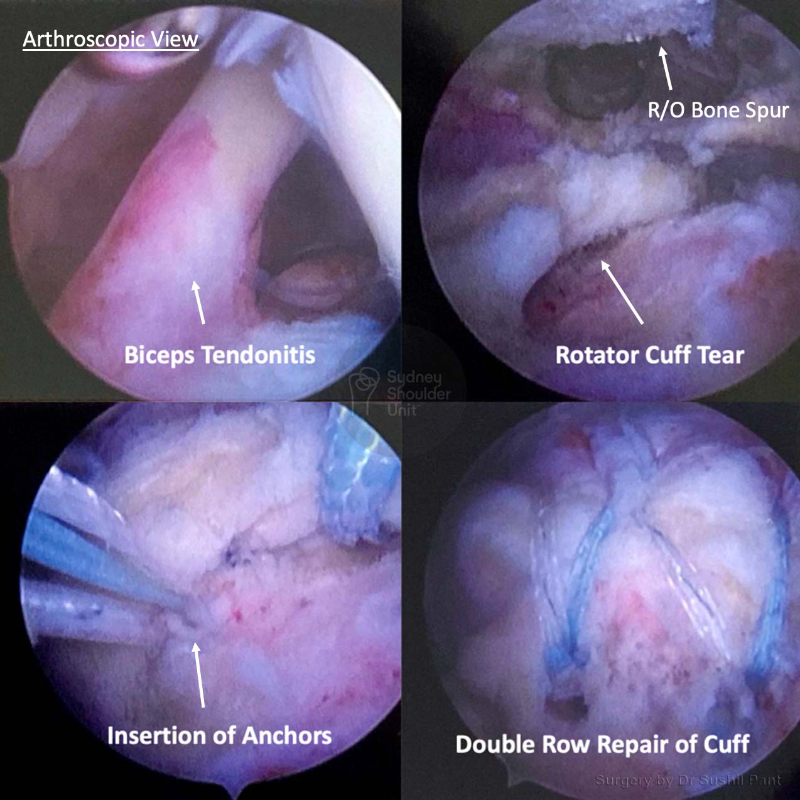
Biceps tendon dislocation (out of the groove).
When the biceps tendon is “subluxed” or “dislocated” out of the groove it can cut into the subscapularis tendon and cause further damage. You should consider surgery sooner rather than later.
Non urgent considerations
Shoudler function
If you are unable to undertake basic tasks or to look after yourself, unable to drive, unable to get dressed, or have difficulty with hygiene and toileting.
Shoudler pain
- Pain with activity and even at rest
- Night pain, especially if it wakes you from sleep
- Unable to sleep on your affected shoulder
- Increasing requirements of pain relief tablets
- Multiple failed cortisone injections
- Not responding to physiotherapy
Work
- If it is limiting your ability to work
- Especially if you are in a manual job requiring repeated overhead activity
Sport
If you are unable (even after a period of rest and activity modification) to participate in your chosen leisure activity or sport and you wish to continue to do so.
Prevent further shoulder damage
There are certain conditions where it may be better to repair your shoulder before further damage occurs. Dr Pant will carefully analyse your MRI scan and determine if this is the case for you (especially in younger patients).