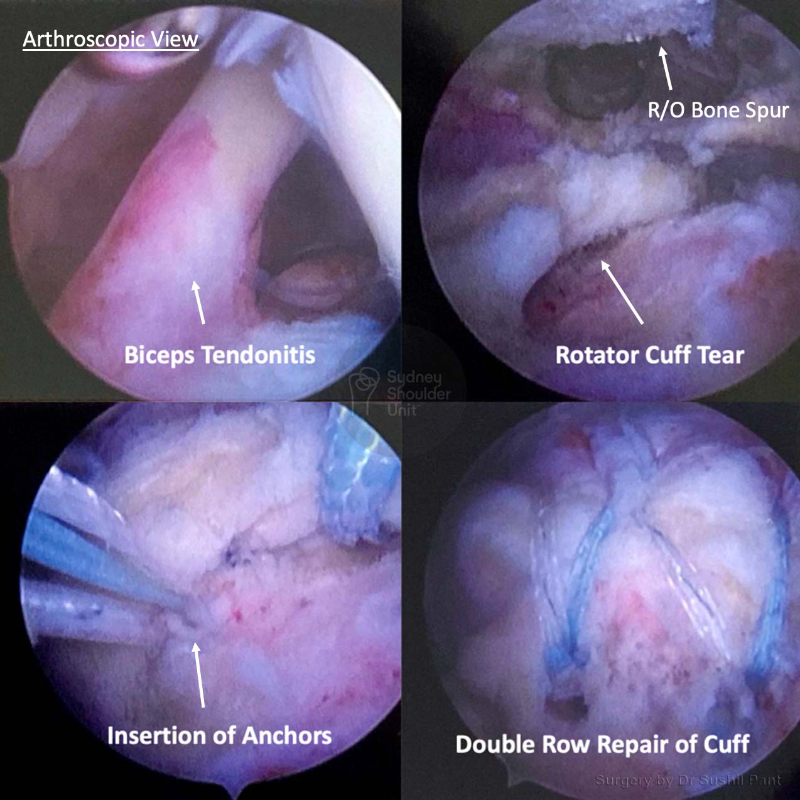
The way to achieve the best outcome after rotator cuff surgery starts with an accurate diagnosis, through patient education, excellent surgical technique, adequate post-surgery pain relief, careful rehabilitation and collaboration with your physiotherapist.
The outcome after rotator cuff repair is generally excellent with the resolution of symptoms and restoration of function. It is not possible, however, to restore the shoulder back to “normal” as your surgeon is using your own tissue to repair what is torn.
There are many factors that contribute to a successful outcome after rotator cuff repair:
- Nature of tear (acute tears do better than chronic/degenerative tears)
- Treatment of associated conditions that may be pain generators (such as the biceps tendon or acromioclavicular joint arthritis)
- General health of the patient
- Quality of the remaining tendon
- Post-surgery compliance with sling use and post-operative protocol
- Physiotherapy
It is important to remember that when performing a rotator cuff repair your surgeon is using your own tissue to repair what is damaged. The weakest point in the repair is usually your own tissue. The longer the history of damage and frequency of trauma prior to surgery, the more likely the tissue quality is poor. Other factors like Smoking and Diabetes may also reduce your tissue quality.
There are three areas where your rotator cuff repair may fail:
Bone-Anchor interface
- The anchors today are very high in quality and usually do not fail; sometimes if your bone is soft (older patients), the anchor may pull out of the bone.
Anchor-Suture interface
This area is typically very strong and not a source of common failure
Suture-Tissue interface
This is the weakest point and the most common reason for failure of surgery (usually due to poor tissue quality)
There are special techniques in tissue management and suture choice to reduce failure rates.
The retear rate of the rotator cuff tendon repair ranges from 5-20% – the larger your tear, the more likely you are to have a retear of your repair. The failure rate after a biceps tenodesis is reported to be between 2-6%; however, in the Sydney Shoulder Unit experience, it is less than 1%.