Surgery is a carefully choreographed process and you are being treated by a sub-specialist shoulder surgeon and a highly experienced team; however, all surgeries inherently carry some risk of complications.
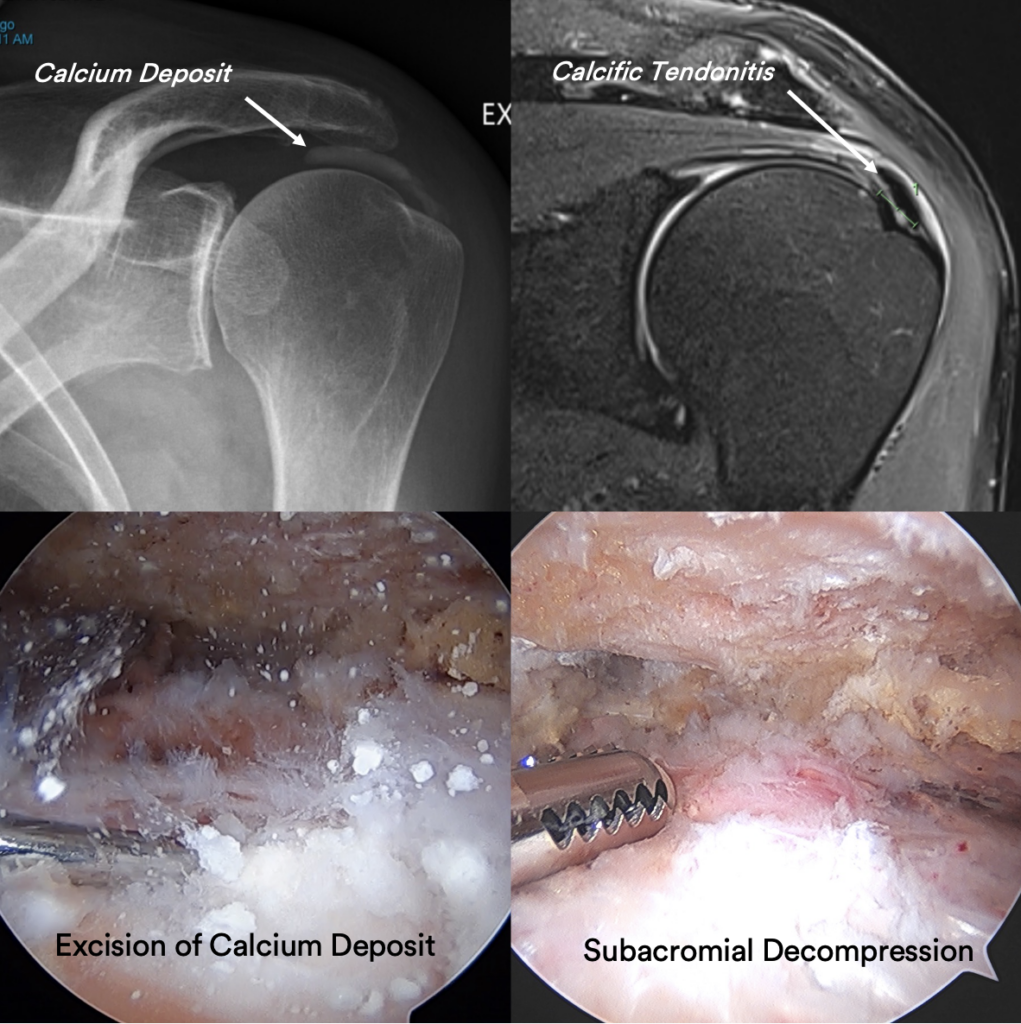
The risk of complications after isolated arthroscopic excision of calcium surgery are less than 1% in the Sydney Shoulder Unit experience.
General risks:
- Infection
- Bleeding
- Wound healing problems
- Damage to blood vessels or nerves
- Sensory changes around the surgical scar
Specific risks relating to Arthroscopic excision of calcium surgery:
- Recurrent of calcium deposit
- Frozen shoulder
Patients who smoke, use tobacco products, have diabetes, or elderly are at higher risk of complications both during and after surgery. They are also more likely to have problems with wound healing.