Patient information
Surgery FAQs
Shoulder surgery FAQ's
Our aim is to educate and empower you and demystify the process around surgery. These Surgery FAQs should answer most of the common questions before and after surgery. Please read through them and ask any further questions during your consultation or call our office on 9215 6100.
When do I need surgery?
Shoulder function
If you are unable to undertake basic tasks or to look after yourself, unable to drive, unable to get dressed, or have difficulty with hygiene and toileting.Shoulder pain
- Pain with activity and even at rest
- Night pain, especially if it wakes you from sleep
- Unable to sleep on your affected shoulder
- Increasing requirements of pain relief tablets
- Multiple failed cortisone injections
- Not responding to physiotherapy
Work
If it is limiting your ability to work, especially if you are in a manual job requiring repeated overhead activity.Sport
If you are unable (even after a period of rest and activity modification) to participate in your chosen leisure activity or sport and you wish to continue to do soPrevent further shoulder damage
There are certain conditions (such a high-grade partial rotator cuff tears) where it may be better to repair your shoulder before tears become full thickness. Dr Pant will carefully analyse your MRI scan and determine if this is the case for youWhat are the costs of surgery?
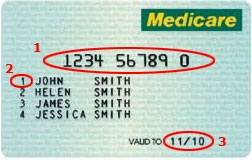
- At Sydney Shoulder Unit we use the AMA (Australian Medical Association) scheduled list of fees as a guide.
- Health Insurance usually pays for your hospital stay and any prosthesis/anchors/equipment that is needed; however, your health insurance only covers a fraction of the doctors’ fees This is because Medicare hasn’t adjusted their rebate to match CPI since 1983.
- Most insurance policies do not reflect the AMA fee, even when they are called “top cover. Most patients have a hospital excess to pay of $500, but it might be different depending on your level of cover.
- If you are not in a health fund then we will provide a separate written quote that clearly outlines the costs associated with your care. Please note that a proportion of the surgical and anaesthetic fee does attract a rebate via Medicare.
- At SSU we take pride in providing clear and accurate surgical quotes. This should go a long way to providing a transparent fee structure and alleviate the uncertainty around the costs of surgery.
What is a medical gap?
Doctors fees
The fees doctors charge patients for their professional medical services must cover their practice costs. Every private practising medical practitioner incurs a wide range of practice costs in order to provide a high quality service to patients. The costs of running medical practices vary across the country, and across speciality groups. But every medical practice, be it a sole practitioner or a large corporate practice, incurs the cost of employing administrative and clinical practice staff, general running expenses such as computers, rent, electricity, professional indemnity insurance and in most cases the cost of medical equipment and supplies. The practice costs must all be met entirely from the fee charged by the doctor for the medical services he/she provides to patients. Source AMA: https://www.ama.com.au/articles/informed-financial-consentHow do I know what time to arrive for my surgery?
- You need to fast for six hours prior to your surgery start time
- The arrival time does depend on which hospital your surgery is booked
- Generally you should arrive at the hospital two hours prior to your start time
- Think of it like checking in to catch an international flight – there are many checkpoints that need to be cleared prior to surgery.
- Please call the SSU staff or Hospital staff if you are unsure or have questions prior to your surgery
When can I drive after surgery?
- It is not recommended you drive while you require the use of a sling
- for simple procedures where the sling is discarded after two weeks – you may then commence driving
- for standard procedures where you require a sling for six weeks – you will be unable to drive for between 6-8 weeks.
How do I have a shower after shoulder surgery?
- You may take the sling off to shower
- Lean forward and allow your arm to “dangle” to wash under your arms
- The dressings applied are waterproof and you may shower with them on
- Usually before you are discharged from Hospital, your dressings are changed after your morning shower.
- These “new” dressings are then kept intact until your review at 10-14 days
- If the dressings start to peel at the edges – you may reinforce them
- When getting dressed, you may use your good arm to move your affected (operated arm) to place your arms through the sleeves carefully
How do I sleep after shoulder surgery?
- Most patients find it difficult to lie flat after shoulder surgery (especially after rotator cuff repair)
- Consider using a few pillows to prop yourself up and sleep at a slight incline; this may be necessary for 4-6 weeks after surgery. You should keep your sling on while asleep
When do I start physiotherapy?
There are three essential components to a good outcome from surgery
- Your surgeon
- You as a patient
- Your physical therapist
Dr Pant utilises the JPL pathway for most patients and this will form the basis of your rehabilitation after surgery; it will be modified to suit your individual circumstance.
The JPL pathway allows for self-directed, early passive shoulder range of movement. The full JPL pathway is available for download.
- Passive = assisted with your other arm
- Active = you move the affected arm independently
Should I change my dressings after surgery?
- Usually before you are discharged from Hospital, your dressings are changed after your morning shower.
- These “new” dressings are then kept intact until your review at 10-14 days
- If the dressings start to peel at the edges – you may reinforce them
- Occasionally you may need to change them if they fall off prematurely or discolour.
What if I think I have an infection?
If the dressings discolour with discharge (yellow or green) you may have a wound infection; do not be alarmed just yet.
Please get in touch with the team at SSU and we will give you a plan.
When will my post operative appointments be?
Close follow up and rehabilitation is essential to a good outcome after shoulder surgery.
First follow up visit (No Fee)
- 10-14 days post operation
- You should still be in your sling
- Dr Pant will review your wound, discuss details of your surgery, the relevant findings, your prognosis, and likely recovery pathway.
- JPL rehab is discussed and physical therapy is commenced.
Second follow-up visit (No Fee)
- Usually 6 weeks post operation
- Discuss the details of your progress to date and any issue that may have arisen
- Most patients will progress along the JPL pathway
- Patients who are not progressing as expected may need a modification of their pathway.
- Some patients may benefit with guidance from their physiotherapist at this stage
Third follow-up visit (No fee)
- Typically 12 weeks post operation
Often the final visit and end of JPL pathway - Most patients at this stage commence strengthening exercises as guided by their physiotherapist.

About Dr Pant
Dr Sushil Pant is a leading Australian trained orthopaedic shoulder surgeon. He is the founder and medical director of the Sydney Shoulder Unit; and is a Shoulder Surgeon at Sydney Sports Medicine Centre at Sydney Olympic Park.
Request a call back
Enquiries between 8am-6pm (Mon-Fri) will be responded to within 30-60 minutes.
"*" indicates required fields
Alternatively, if you have any further questions or would like a consultation with Dr Pant get in touch: