Subacromial bursitis commonly causes local swelling and tenderness over the side and front of the shoulder. Patients often report pain, pinching, or stiffness when lifting their arms. There may also be a pain when the arm is lowered from an elevated position.
Initially, the symptoms are often mild and tolerable – in such cases patients do not often seek treatment.
These symptoms of Subacromial Bursitis are typically:
- Pain that is present with activity and rest
- Pain radiating from the top of the shoulder (either at the front or the side) down the side of the arm
- Sudden pain with reaching or lifting movements
- Overhead athletes may report pain with particular actions (such as a tennis serve or throwing a ball)
As the condition progresses the symptoms may worsen and not respond with periods of rest and activity modification:
- Night pain (particularly waking you up at night)
- Inability to lie on the affected side at all
- Reduced strength and range of motion
- Difficulty with activities that require the arm behind the back – such as buttonon, zipering, putting on bra etc.
When the symptoms persist and affect your quality of life then it is important to seek review.
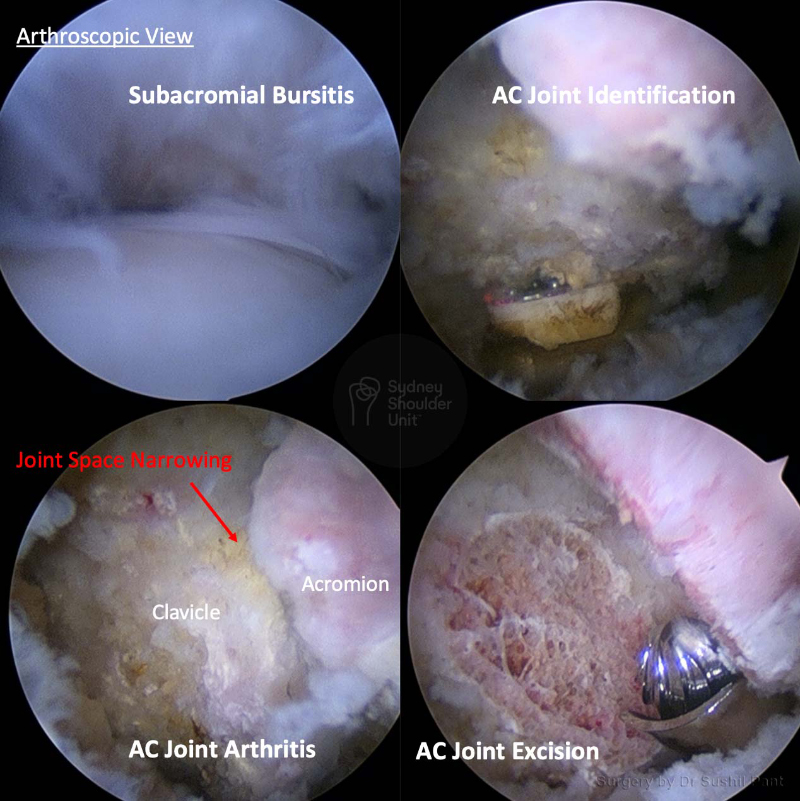
Examination
A thorough examination of the shoulder is required, including checking areas of tenderness, range of motion, associated pathology (such as biceps tendon or rotator cuff tears) and then special impingement tests to isolate the subacromial space.
Imaging
A plain X-ray will often show a spur under the acromion, and in some cases, there may be an exaggerated curve under the acromion (a type 2 or type 3 acromion). Patients with type 2 or 3 acromion are at increased risk of shoulder impingement and tendon tears.
MRI will show the soft tissues in greater detail and demonstrate any fluid or inflammation in the bursa. It will also show the rotator cuff and biceps – looking for any partial or complete tears.